Nowadays in the UK the most common reason for itch is allergy & the most common allergy if canine atopic dermatitis & the feline equivalent – atopic skin syndrome…
Allergic reactions, or hypersensitivities, occur when an individual’s immune system reacts inappropriately to a normal substance in the environment. These substances, or allergens, include flea saliva, dietary protein and aeroallergens. The immune system mistakes these allergens for an infectious agent. The reactions occur when the allergen contacts the skin, is eaten or is breathed in. The allergen is recognised by specific antibodies, these combine with various cells, these cells produce a cascade of many chemicals that produce inflammation. With skin allergies this inflammation causes itching. The most allergic dogs and cats have one, or a combination of these three conditions: Flea Bite Hypersensitivity, Cutaneous Adverse Food Reactions and Atopic Dermatitis (aeroallergens).
The latter condition is the most common cause if pruritic (itchy) skin disease in the UK dogs. Conservative estimates are that 10% of the canine population suffer with atopic dermatitis to some degree. There are many similarities with human atopic dermatitis (atopic eczema) but also some notable differences – dogs do not grow out of this condition, as do a significant proportion of children, but many of them do respond to allergen-specific immunotherapy (ASIT). Atopic humans do not respond well to ASIT but those with allergic rhinitis (hayfever) or insect venom hypersensitivity do.
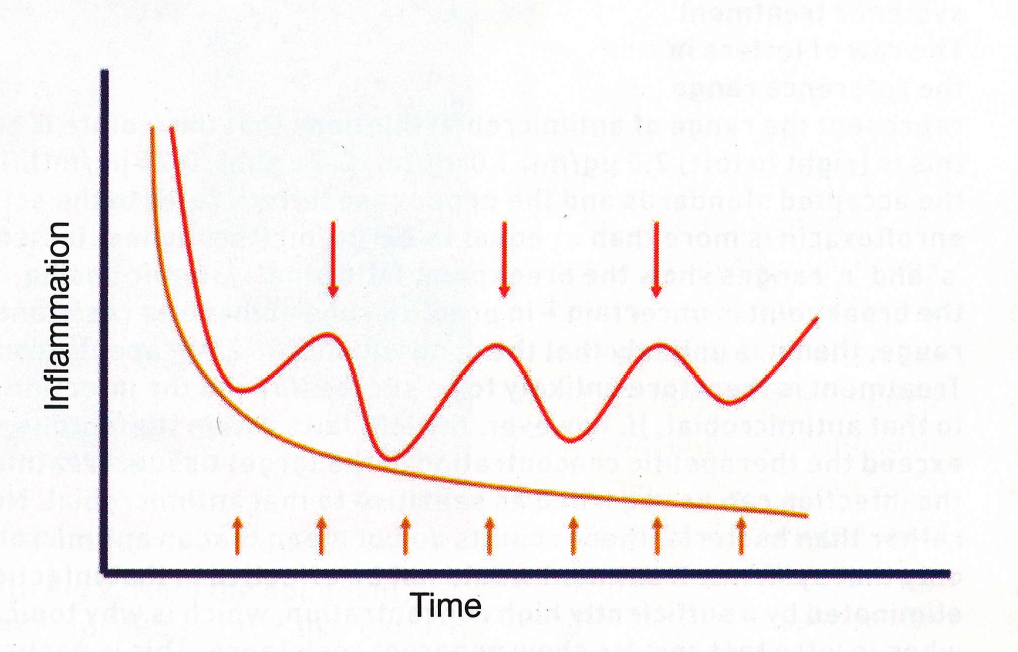
Successful tong-term (pro-active) management of atopic dermatitis, requires ongoing, regular, anti-inflammatory treatment to maintain remission and prevent relapses especially secondary microbial infection (bacteria and/or yeast). Such proactive therapy [the lower orange line with regular orange treatment arrows] gives much better control and improved quality of life, which in the long term is also cheaper for the client. Whereas treatments given for each bout of infection (reactive) gives short-term relief, but ignores the ongoing inflammation [the upper red line with irregular red treatment arrows]. Reactive management will result in chronic inflammatory changes causing more frequent and severe infections. This approach actually results in the use of higher doses of, and total amount of, anti-inflammatory drugs increasing the possibltiy of side effects. It reduces the pet’s quality of life, increases the number of visits to the vet and ultimately costs the owner more time and money. Additionally the increased use of oral antibacterial courses encourage development of resistant skin microbes.
Successful Long Term Management of Canine Atopic Dermatitis
I will outline a pro-active, long term treatment regimen¹ for each individual allergy case I am referred. A tailored, dynamic sequential and multi-modal management plan is needed for each individual dog throughout their left stages & the evolution of their condition. The management & treatment plan will include advice on:
oral or topical ectoparasite control – dependent on previous and likely future exposure; number & species of in-contact domestic pets, lifestock and wildlife; confirmed, or putative, concurrent flea bite hypersensitivity http://www.theskinvet.net/downloads-links/372-2/
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
http://www.theskinvet.net/clients/recurrent-ear-infections/
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
http://www.theskinvet.net/clients/immunotherapy-for-atopic-pets/
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
¹I have complete clinical freedom from corporate practice-prescribing constraints.